An excerpt from the 2024 Family Medicine Update Oct. 23 – 25.
Early Onset Colorectal Cancer
Colorectal cancer (CRC) isn’t found just in older adults anymore. Early onset colorectal cancer in those under age 50 is in the top five ranking cancers connected with high disability-adjusted life years, combining years of life lost due to premature death and years lived with a disability. Dr. Fritz recently talked on how early onset CRC needs better awareness, quicker diagnoses and more prevention strategies that work.
Recognizing the Warning Signs
Symptoms of early onset CRC can appear months or even years before diagnosis. These can often overlap with other less severe conditions. Common symptoms include:
- Abdominal pain: Often dismissed as indigestion or other minor issues.
- Rectal bleeding: A major warning sign and highly associated with CRC, though it’s sometimes mistaken for hemorrhoids.
- Diarrhea: Persistent diarrhea shouldn’t be ignored.
- Iron deficiency anemia: A shortage of iron in the blood, which can cause fatigue and weakness, often goes undetected but can be a critical indicator of CRC.
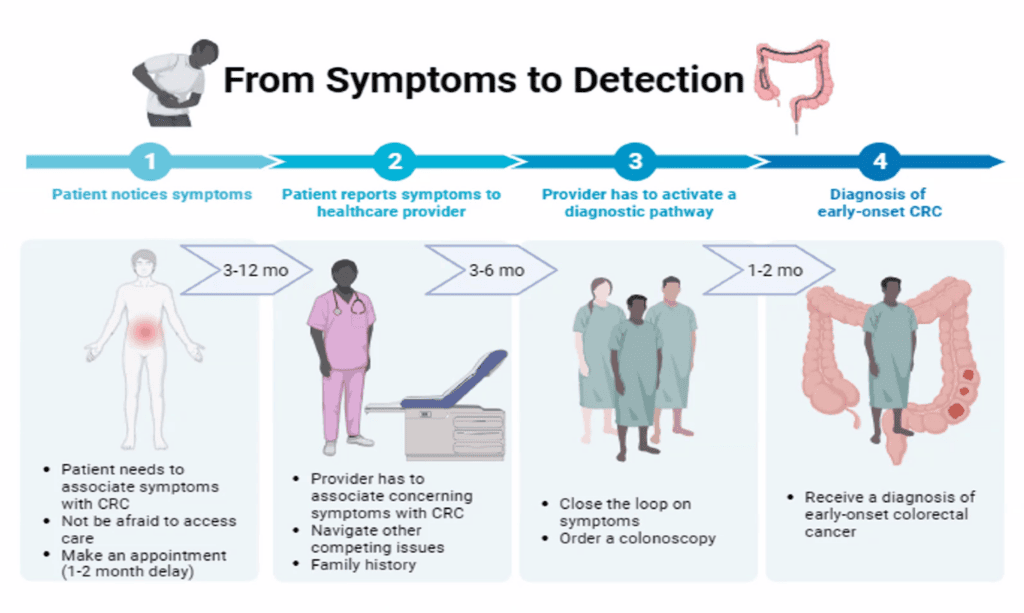
Dr. Fritz said these symptoms can appear up to 18 months before a CRC diagnosis. However, these signs are often overlooked or misdiagnosed because they are similar to less serious issues. This leads to dangerous delays in diagnosis and treatment, especially among young patients who might not consider themselves at risk.
Risk Factors for Young Adults
While genetics play a role in CRC risk, Dr. Fritz emphasized that only a small percentage of early onset cases are due to known genetic factors. This means that lifestyle and health factors are significant contributors. Key risk factors include:
- Unhealthy diet: Diets high in processed foods, fats and red meats.
- Lack of physical activity
- Type 2 diabetes
- Excess liver fat
- Alcohol consumption
By managing these factors—through diet, exercise, and moderating alcohol intake—young adults can help reduce their risk of early onset CRC. However, these lifestyle changes must be combined with increased awareness and screening.
The Problem of Late Diagnosis
One of the bigger challenges with early onset CRC is late diagnosis. Young adults are less likely to screening, especially since the official screening age was set at 50 until recently. Now, the screening recommendation has been lowered to 45, but Dr. Fritz argues that even this change isn’t enough. More than half of early onset CRC cases occur in people younger than 45, meaning many young adults are still unlikely to be screened before symptoms appear.
The traditional screening tool for CRC is a colonoscopy, but colonoscopies are invasive, require specialized equipment, and travel can hinder especially in rural areas where access ess can be limited. Dr. Fritz said stool-based testing is a more accessible and practical option. These tests, such as the fecal immunochemical test (FIT) or Cologuard, can identify CRC early. While not as thorough as a colonoscopy, they offer a non-invasive alternative that could help reach a broader population, especially young adults.
Preventing Colorectal Cancer: What Can Be Done?
Preventing CRC requires a two-fold approach: regular screening and managing lifestyle factors. Many risk factors for CRC can be tackled with healthier choices, such as diet, activity level and drinking alcohol. Dr. Fritz also discussed the potential role of aspirin and nonsteroidal anti-inflammatory drugs (NSAIDs) in preventing CRC. Recent studies suggest that using NSAIDs two times a week might reduce the risk of developing certain types of high-risk villous adenomas, which are more likely to progress to cancer. While more research is needed, these findings hint at NSAIDs playing a larger role in preventing CRC.
Increasing awareness is also crucial. Young adults may not realize they are at risk, and symptoms like abdominal pain or rectal bleeding may not immediately prompt a doctor’s visit. Dr. Fritz said that educating young adults about CRC symptoms is vital. The more people know, the more likely they are to seek help early.
Primary care providers are the front line of CRC detection. PCPs should discuss CRC risk with patients during any medical visit, not just during annual checkups. Regular conversations about CRC screening can increase the chances that a patient will eventually agree to be tested.
Unfortunately, in low-resource areas or regions with a shortage of healthcare providers, access to CRC screening is often limited. Dr. Fritz noted that the shortage of colonoscopy providers, particularly in rural areas, emphasizes the need for alternative options like stool-based tests. By promoting these alternatives, PCPs can help close the screening gap and catch more cases early.
Moving Toward a Healthier Future
Dr. Fritz believes that lowering the screening age is a positive step but only part of the solution. She wants a more flexible approach where stool-based testing becomes a primary option for younger patients and those in under-resourced areas.
In addition, she stressed the importance of knowing family medical history. A family history of CRC, especially among first-degree relatives, is a major risk factor and should prompt earlier screening.