An excerpt from the Family Medicine Update Oct. 23 – 25, 2024.

What Is COPD?
COPD covers several lung conditions, most commonly chronic bronchitis and emphysema. COPD develops primarily from smoking or long-term exposure to harmful substances such as air pollution, dust and industrial chemicals. Around 400 million people suffer from COPD globally, 10% in the United States. COPD costs the U.S. healthcare system $40 billion annually and is one of the leading causes of disability and death.
Risk Factors for Developing COPD
More than 70% of COPD cases in the United States is from smoking. However, other factors also contribute:
- Exposure to indoor and outdoor pollution: This includes fumes from cooking fuels, industrial dust and air pollution.
- Occupational hazards: Working in environments with dust, chemicals or fumes without adequate protection.
- Genetic predisposition: Some people are genetically more susceptible to developing COPD, meaning they might develop the disease even if they smoke less than others.
- Childhood health factors: Premature birth, childhood infections, poverty and malnutrition during developmental years can increase COPD risk later in life.
Symptoms and Types of COPD
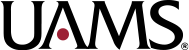
COPD presents differently in each patient, but common symptoms include shortness of breath, chronic cough, excessive mucus production and fatigue. COPD is sometimes classified into two main “phenotypes”:
- Chronic bronchitis: Patients experience inflammation in the bronchial tubes, increased mucus, and frequent coughing.
- Emphysema: This form involves damage to the alveoli in the lungs, reducing oxygen exchange.
There are also other variations of COPD, including overlap with conditions like asthma, bronchiectasis (permanent airway widening), and pulmonary fibrosis (scarring of lung tissue). Each type requires specific treatment based on the severity and the symptoms experienced.
Pathophysiology: How COPD Affects the Lungs
COPD damages both the airways and the alveoli. In healthy lungs, airways are clear and elastic, allowing smooth airflow. But in COPD patients, irritants such as cigarette smoke cause inflammation, smooth muscle thickening and mucus buildup. These changes block airflow, which can trap air in the lungs, making it harder to breathe. Alveoli can also become damaged, leading to fewer blood vessels and reduced oxygen exchange. This complex damage results in mild to severe symptoms, depending on how much of the lung is affected.
Diagnosis of COPD
Doctors diagnose COPD based on symptoms, history, and lung function tests like spirometry. The most common measurement is the FEV1/FVC ratio, which compares the amount of air a person can exhale in one second (FEV1) to the total amount exhaled (FVC). A ratio below 0.7 usually indicates COPD. However, the severity can vary, and some patients with COPD symptoms may not fit this strict diagnostic ratio. Doctors also assess how far along the disease has progressed by examining how the symptoms impact a patient’s quality of life.
Updated Guidelines for Managing COPD
The Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines are the leading reference for managing COPD. GOLD recommends a staged approach to treatment based on symptom severity and frequency of exacerbations (flare-ups):
- Group A (few symptoms, low risk of exacerbation): These patients typically manage with a bronchodilator to ease breathing.
- Group B (more symptoms, low risk of exacerbation): Initial treatment usually involves a combination of long-acting bronchodilators.
- Group E (high risk of exacerbations, more symptoms): This group often requires a combination of medications, sometimes including inhaled corticosteroids.
The GOLD guidelines have recently combined the former Groups C and D into the new “Group E” category to simplify management. Patients in Group E, who often have frequent exacerbations, may need a more aggressive treatment approach to prevent hospitalizations and further lung damage.
Treatment Options for COPD
The primary treatments for COPD involve medications delivered through inhalers or nebulizers. These include:
- Bronchodilators: Drugs that relax the muscles around the airways, making it easier to breathe.
- Inhaled corticosteroids: Used mainly for patients with frequent exacerbations, these reduce lung inflammation.
- Triple therapy: This combination of bronchodilators and corticosteroids is recommended for patients with severe symptoms and frequent exacerbations.
In addition to medication, lifestyle changes such as quitting smoking are critical for slowing COPD progression. Smoking cessation can drastically slow lung function decline, allowing patients to maintain a better quality of life.
Non-Drug Treatments for COPD
Dr. Deas emphasized that several non-pharmacological treatments can have a significant impact on COPD outcomes:
- Pulmonary rehabilitation: Exercise and education programs help improve lung function and reduce hospital visits.
- Oxygen therapy: For patients with low oxygen levels, this therapy can extend life expectancy if used regularly.
- Immunizations: Vaccinations against flu, pneumonia, and COVID-19 help protect patients from respiratory infections that could worsen COPD symptoms.
For some patients with very advanced COPD, newer treatments like endobronchial lung volume reduction (ELVR) surgery might be an option. In this procedure, doctors place small valves in the lungs to block airflow to the most damaged areas, allowing healthier parts of the lung to function better.
New Treatments and Future Directions
Recent studies have introduced new treatment options that may benefit certain COPD patients:
- Dupixent: Originally used for asthma, Dupixent is a biologic medication that may reduce exacerbations in COPD patients with elevated eosinophil levels (a type of white blood cell).
- Ensifentrine: This new inhaled medication has shown promise in improving lung function and reducing exacerbations in patients who continue to struggle with standard treatments. Though expensive, it represents an advancement in COPD treatment.
The Importance of Ongoing Monitoring and Support
Effective COPD management requires more than just prescribing medication. Patients often need regular check-ups to monitor their symptoms, adherence to inhaler techniques, and any side effects from medications. Adherence to inhaler use can be a particular challenge for COPD patients, so respiratory therapists or nurses can help patients learn the correct technique. Video tutorials and in-person coaching can also help improve inhaler use and medication effectiveness.
COPD as a Multi-Organ Disease
Finally, Dr. Deas highlighted that COPD impacts more than just the lungs. The disease often leads to inflammation throughout the body, which increases the risk of heart disease, osteoporosis and frailty. Providers treating COPD patients should consider these broader health risks and encourage patients to adopt a well-rounded approach to health.