In the summer of 2016, Stuttgart native Blake Pond, 36, moved back to his home state after living in Dallas for 16 years. He, his wife, Ann, with their infant daughter, Caroline, wanted to be closer to family. So Pond accepted a position as chief of staff at the UAMS Myeloma Institute.
On Oct. 5, 2017 a day before Caroline’s first birthday, Pond scheduled an appointment with Chuck Smith, M.D., at the UAMS Rahling Road clinic to establish primary care.
“I told him I’d been having some symptoms over the past couple of years,” Pond said. “I just thought to mention it. But that piece of information along with my family history concerned Dr. Smith, who recommended to get it checked out just to be on the safe side.”
Smith referred Pond to get a diagnostic colonoscopy which revealed a polyp about the size of a golf ball. He was diagnosed with invasive adenocarcinoma of the colon, the most common type of colorectal cancer.
The news came as a surprise to Pond.
“I’d been in oncology research for 10 years, so all these thoughts were going through my head. The worst part was the unknown,” he said.
Conan Mustain, M.D., a board-certified colon and rectal surgeon and assistant professor in the Department of Surgery, talked through the next steps with Pond.
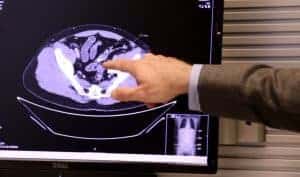
“First we got a CT scan to look at his lungs and liver,” Mustain said. “Those are the two sites most common for colon cancer to spread.”
Blake’s scan came back clear. There was no evidence that the cancer had spread.
“The decision then was whether removing just the polyp was adequate treatment or if we needed to also remove part of the colon,” Mustain said.
Mustain said there were two things to consider when it came to deciding whether to remove a part of Pond’s colon: the polyp site itself and whether cancer had spread to the regional lymph nodes. For some early cancers the risk of lymph node spread is sufficiently low that complete removal by colonoscopy is considered adequate treatment. In Pond’s case pathologists had not been able to confirm if the base of the polyp’s stalk (a piece of tissue that attaches the polyp to the intestinal wall) was completely clear of cancer. Additionally, some enlarged lymph nodes were visible on his CT. Given his young age, uncertainly about these nodes could mean years of costly surveillance and worry. Pond and Mustain ultimately decided they’d remove part of the colon and the lymph nodes.
The surgery was scheduled for Oct. 30. Mustain laparoscopically removed 10 inches of Pond’s colon containing the polyp site and 16 regional lymph nodes. The minimally invasive approach included three small incisions around the abdomen. Mustain says doing the procedure this way leads to less pain, lower narcotic use and a faster return to normal bowel function after surgery. Pond was discharged from the hospital after two days and back to work in two weeks.
“I’m grateful for the whole health care team at UAMS,” Pond said. “From Dr. Smith for having the wherewithal to refer me for a colonoscopy to my follow-ups after surgery. I really think this is a good example of the system working. My original primary care appointment was Oct. 5. By Nov. 5, I was back on my feet and on the road to the recovery.”
Pond went on a ski trip in January and performed at a level he would have prior to his diagnosis and surgery.
“No one is eager to get a colonoscopy,” Pond said. “But you have to know your body and if there are any symptoms, don’t wait to get it checked out.”
Mustain says colon cancer screening should begin at age 50 for most people. Those tests should come sooner if a patient shows symptoms or has a parent, sibling or child who was diagnosed with colorectal cancer.