
Introduction
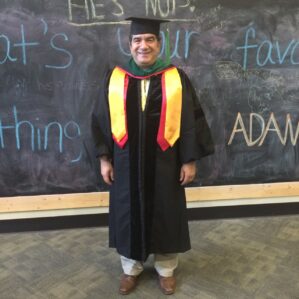
Our first mentor we cannot wait to introduce you to is Dr. Hakan Paydak of the Cardiology Division of the Department of Internal Medicine. He is well known to our medical students as he teaches an amazing EKG course for M4s! Listen to this first episode of Mentor Spotlight to learn more about Dr. Paydak’s journey through medicine and to UAMS, his interests, as well as his advice for students.
Episode Transcript
Manasa: Welcome to the first episode of Mentor Spotlight, a podcast designed to help connect UAMS medical students to faculty mentors. We are Manasa, Hannah, and Weijia, your hosts for this episode. Today, we have Dr. Hakan Paydak, an Electrophysiologist in the cardiology department at UAMS.
Hannah: Originally from Turkey, Dr. Paydak was an Assistant Professor of Medicine at the Medical College of Wisconsin before he joined the UAMS COM in 2009. He started the cardiac electrophysiology program as well as Device Clinic here. He is also highly active in research, publishing over 80 pieces to date and has presented at over 105 conferences.
Weijia: He also teaches the fourth year class “ECG Reading and Arrhythmias”, highly recommended by those who take it. He has won over 10 teaching awards nominated by medical students, residents, and fellows.
Manasa: Without further delay, let’s talk to Dr. Paydak. Hi Dr. Paydak, we are excited to have you here being our first faculty mentor being spotlighted!
Dr. Paydak: Thank you
Manasa: Everyone that knows you has wonders to say about you, so it is high time everyone learns about you and how you want to get involved with students!
Dr. Paydak: Sure
Manasa: Can we start off with you telling us a little bit about yourself?
Dr. Paydak: Sure. I was born and raised in Turkey. I was born in St. Paul’s City of Tarsus and I lost my dad at five years of age so it was a hardship for me. But I think it made me stronger in life later on. At 11 years of age, I went to a boarding school in Istanbul, which is the biggest city in Turkey and had all of my classes in English and some in German by American teachers and English teachers. It was a private school designed specifically for the kids who had lost their fathers in the wars. I became a part of the school and I still keep my relationship with the school. We are actually going to be celebrating our 40th graduation anniversary this June and I’ll be staying at the school for one night. It is one of the top schools in the country and after graduating that school as the valedictorian, I had a brief stint in the United States as an exchange student before I graduated. When I was a Junior in my own high school, I came to the United States as a Senior high school student and stayed with an American family, whom I call mom and dad, Mr. and Mrs. George and Karen Marshall, who I’m gonna visit this weekend in Phoenix, Arizona. They hosted me for a year and that was one of the best years I have spent in my life because I came from a boarding school and then saw that people were coming to school by driving which was a big big change for me. I had a wonderful year and I still call my mom and my dad. They are gonna put me on their will. They said they saw my home here and they said “We are taking you off the will,” but that’s okay. My dad was a hall of famer in basketball in Indiana, so he told me he is gonna give me his trophies.
Everyone: *laughing*
Hannah: That’s a pretty good inheritance, if I do say so myself. Alright, if you wouldn’t mind, you told us about your upbringing, what made you specifically decide through your medical journey that you wanted to specialize in cardiology and then even more specifically in electrophysiology.
Dr. Paydak: So that’s a great question. So my uncle was an internist and my other uncle was a dentist, so they were both in the medical field. My uncle who was an internist was a great physician in my opinion and I worked with him in middle school years during summer time. I helped him register his patients and there were about 65 of them a day. And he was very caring, he didn’t even go to lunch. He started early in the morning and stayed very late. He took care of the patients. Some patients couldn’t pay him, but they would bring him some chickens or some other gifts, etc. So he was my role model. He was also very interested in cardiology but then during the second year of medical school, I went to Hacettepe University School of Medicine in Ankara, Turkey, which was a top medical school in the country and I am one of the first graduates from the English group. During my second year of medical school, I got sick during summer time. I was doing translations, I was trying to become a tourist guide to make money and I was interested in tourism and could use my english. But then I think I over worked, I was also doing some research in biochemistry and I think I overworked and I had a viral pericarditis, myocarditis involvement and I almost died. But they did a cut down and they took me emergently to the hospital and I survived, thank God. But this made me more interested in cardiology. And then after finishing medical school, I went to study internal medicine in residency, but I wasn’t always determined to go into cardiology. What happened was, I got lucky. In the middle of my residency after the second year or so they said cardiology is now going to be a different department and the ones who wish to go into cardiology can apply and if they are chosen then we are automatically going to let them finish, do three years of cardiology fellowship and that was a great opportunity for me. So I didn’t need to take any extra exams or anything like that to go into cardiology. And then I was reading a lot, I was reading a pamphlet on the wall one day during my residency and I saw that there was a scholarship from the Netherland’s government to do research in the Netherlands at one of the top centers. And I applied for it and I got chosen and I spent a year in the Netherlands and worked on cardiac electrophysiology and I didn’t know anything about cardiac electrophysiology until I went to the Netherlands. It was a virgin field in Turkey and this is happening in 1992, so this is about 30 years ago. I chose to go into clinical cardiac electrophysiology or heart rhythm disorders because mentor said this is the only virgin field in Turkey, and I know you want to stay in academic medicine, so if you chose this field, he said, then your chance of staying in academic medicine will be higher. So I did a proposal for research and it was accepted and I went to the Netherlands for a year and worked at Utrecht University Hospital for a year and was clinical cardiac electrophysiology fellow. I worked with one of the top cardiac electrophysiologist in Europe at that time. The physicist that worked in the group at the time, actually invented the mapping systems that we are using today and had 40 patents. And my boss there, he later died, Professor Robles de Medina was so kind, he told me that if they liked me they would give me the second six months of scholarship and they paid me actually three times the scholarship that I received in the first six months from the Netherland’s government and they gave me an extra 500 euros to go on vacation. So it was a great year there and that expanded my chance of coming to the United States because, had I not had one year of training in cardiac electrophysiology at one of the top centers in Europe, I don’t think that I would’ve been able to come to the United States by phone interview. So after I finished my cardiology fellowship, I was offered to stay as chief of cardiology at a smaller university hospital in Turkey, but I decided to pursue electrophysiology, because at that time electrophysiology, and still is, very expensive, so it isn’t one of the fields that is actively pursued by people in Turkey. So I thought that I should come to the United States for further training. So I applied to positions and Dr. Richard Kehoe from Illinois Masonic Medical Center in Chicago asked me for an interview and I said I don’t have enough money to come and visit you but can we do it over the phone? He said yes. Because of my prior training in the Netherlands he thought that I would be a good candidate and he offered me the job, I accepted it. When I came I told him, I have not been to the United States over the last 16 years, I was there as an exchange student but I don’t know anything about Chicago. And when I came to the airport, I might be the only fellow, who… there was a limo waiting for me, at the airport for me. He was so kind, he provided the limo, he provided a furnished apartment for me until I got my stuff and I started working as an electrophysiology fellow with him and his group. On the third day, he invited me to his home and said “look we want you to stay for another year, if you want you want to do another year” and I said “look let me apply to ten best places in the country and if I get in, I’ll do a year there, if I don’t then I’ll do another year here with you.” He wrote me very nice letters and I ended up working for his rival, University of Chicago, in Chicago. So that was that was the best training that I’ve had at one of the top schools in the country and I worked with one of the best electrophysiologists in the world, Dr. David Wilbur and I published a circulation paper in 1989 and I want to go back to Turkey and work as an electrophysiologist, but the opportunities were still not there at the time, so I decided to go to Kuwait. Because it was closer and there was an electrophysiology opportunity. But then they told me that I need to be board certified in the United States in order to work in Kuwait, so I said “I am getting board certified.” In addition, I interviewed at the University of Illinois, but I couldn’t get the job because I don’t have a license, I don’t have any board certifications, none of those things so they couldn’t offer me the job unfortunately. So I said “I am going back to training.” That was the moment difficult year of my career in the United States because I went from PGY-8 at the University of Chicago to PGY-1 at Illinois Masonic Medical Center. When I was a fellow there, the interns who worked with me became my residents, the residents became my attendings. But still, I had a great year. They made me run the EKG courses there for the morning report because of my EKG knowledge and cardiology knowledge. And I did research with Dr. Kehoe and the group. I did my clinic with him and the board gave me a year of credit because of my prior training in Turkey, so in two years I became an internist. I then decided to apply for a cardiology fellowship. I couldn’t convince Northwestern University that I would get a year of credit, but Case Western was convinced that I would get it. Case Western offered me a position out of match and I accepted it. There I worked with Dr. Waldo and the group over there. Dr. Waldo is one of the most pioneers of electrophysiology. So I have been lucky to have great mentors in my life and I think this helped me to become a good teacher, because I learned from all these wonderful mentors.
Weijia: That’s a great story, thank you Dr. Paydak. So I’m gonna take us back a little. When I first heard the word ‘electrophysiology,’ I was like ‘something fancy to do with the heart’ right. So could you explain to us maybe what you do on a daily basis.
Dr. Paydak: Sure. So electrophysiology means studying the electrical components of the heart. The heart composed of two parts, one of them the plumbing that supplies the blood supply to the heart. The other one is electrical system that helps the heart contract 72 beats per minute most of the time. Electrical problems can be due to slow rhythm problems or rapid rhythm problems. For the slow rhythm problems, we will implant pacemakers, like I did on Wednesday, to a patient who needed a pacemaker. For the rapid rhythm problems that can potentially kill you, then we can implant a defibrillator. Which can detect the rhythm problem and pace you out of it or shock you out of it and that’s what I did today at the VA medical center. We implanted a defibrillator with two leads. So there were two reasons I went into this field, one of them is: it is very rare in medicine to be able to cure things, but in electrophysiology, your heart rhythm disorders, there are chances for us to be able to cure things by procedures. One of them is ablation. Ablation is through the tip of a catheter, we can pinpoint the cause of the rhythm problem and we can burn there, without causing any damage to the patient, eliminating the rhythm problem for good. For instance, for patients with Wolff Parkinson White there is an extra connection between the upper and lower chambers and if you pinpoint that and eliminate the problem the patient will not need to be on medications for the rest of his or her life. This is the main reason why I went into this field. The second reason was to be able to prevent death in people that are prone to having rhythm problems that can potentially kill them. By implanting a defibrillator, we can save their lives and the defibrillator will get them out of abnormal rhythm problems and save them. I’ve seen many patients who have survived with the defibrillators I’ve implanted over the last 30 years.
Manasa: So you have had quite the bit of journey to where you are now. So currently, what job positions do you hold within UAMS here.
Dr. Paydak: So I’m a professor of medicine since 1995. I am the director of the electrophysiology lab and electrophysiology fellowship program since I came here 13 years ago, since 2010. And I became the associate chief of the Division of Cardiology in 2017 and I also member of the promotion and tenure committee for the university, for the College of Medicine. These are the main positions that I hold, for now.
Manasa: That’s more than enough
Hannah: That’s perfect. It sounds like you have done a lot of research in your training leading you here. Are you currently doing any research or have any particular research interests?
Dr. Paydak: Yes. We are actively doing research with our students, medical students, with our residents, and with our fellows, both cardiology fellows and EP fellows. I was just talking to one of our medicine residents who interested in going into pulmonology. One of the things we want to look at is, we use amiodarone most of the time, short term. It’s the most effective medication we have, but it does have a lot of side effects. So I was just suggesting we can look at the amiodarone related side effects over the last 13 years I’ve been here and we can especially look for the lung related side effects, since he wants to go into pulmonology, for instance. We have published recently a report on using the graphic trends for differentiating supraventricular, ventricular tachycardia and this is a special project for me because we utilized our senior medical students that rotate with me for this EKG course and arrhythmia course. They became our subjects. So what we did was, we asked them to look at the telemetry of the patients to detect whether the patient is having supraventricular tachycardia and what type is it. Is it a sinus tachycardia, meaning the normal heart beating faster and faster like when we exercise. Or is it a sudden onset, sudden offset rhythm problem. And just by looking at the telemetry they were not sure, but then when we looked at the graphic trends they showed us whether there is a sudden increase in the heart rate and it will be in the shape of a rectangle or a square versus whether there is a gradual increase in the heart rate and gradual decrease in the heart rate that will be a bell shaped curve like when we exercise. So after looking at those graphic trends, their accuracy increased to better than 95%, for fourth year medical students. This is a paper that our chief, one of our cardiology fellows right now is the first author, I’m the senior author. So I’m very proud of this paper because we got our senior medical students involved as well. And we are doing mostly clinical research and we have done some research that is dedicated to UAMS patients only and we have published them. We have also done some database driven research and we have had publications and circulations and etc. So we are currently doing both clinical research and database driven research with our fellows.
Manasa: And can medical students get involved and reach out to you if they are interested?
Dr. Paydak: Absolutely! Absolutely! So, I have to tell the story of one of our phenomenal residents who came to me as a first year medical student. She said she would like to do research with me and we did a paper together on utilization of rhythm controlling medications in pregnancy. She was the first author and I’m the senior author. She wanted to go into cardiology, but then she got married and now she is gonna work as a faculty in internal medicine at North Little Rock Baptist Hospital. I’m sorry that she’s not gonna go into cardiology but this is an example of one of our medical students, first year medical students, has published a paper with us. And one of our other medical students that did research with me is now a cardiology fellow actually, he is gonna be graduating from our program. So we get our medical students involved and also we get Dr. Mehta, Jay Mehta, who is our research guru involved with our research projects and get his input as well.
Weijia: That’s really good to hear. Personally, I have been having some trouble finding research, so I’m glad doctors are open to med students. Aside from research and your job, I was curious what are some of your passions outside of the hospital?

Dr. Paydak: Oh, I am a big sports fan. I played soccer in my youth on my high school team and also ameatur soccer in Turkey and one year in the Netherlands. When I was an electrophysiology fellow, I played soccer in the Netherlands. And then I ran cross country in the U.S. because when I came to the U.S. as an exchange student, my high school unfortunately did not have a soccer program. So they asked me to become the kicker of the football team. So the first time I am trying to kick, I am kicking and the guy that is the holder isn’t very happy and I said ‘What’s wrong’ and he said ‘Can you try and kick it a little bit higher’ because I was kicking under the bar, like soccer style. So when I started to kick it over, I became their kicker and since then I have a great passion for American Football, soccer, both my kids play soccer, and one of them is playing basketball now and the other one is at college now, at UC Berkeley, he is playing intramural soccer with some Turkish kids there, that he met over there. So sports is my biggest out of hospital hobby. The other one is playing chess, again with my kids and also I have been playing for years. It gives you an advantage of troubleshooting and analyzing, etc. so I would advise any student to learn to play chess and then to play it. And traveling, you know we go to Turkey every year to visit my family, but we have also traveled in Europe and I had a couple of clerkships during my medical school years actually, one year in the Netherlands, one year in Denmark, one year in former Yugoslavia. As a matter of fact, I saw my first pacemaker implantation when I went there for a clerkship at the end of my fourth year of medical school, in Yugoslavia.
Manasa: That’s awesome!
Dr. Paydak: I just said ‘this is very nice, very interesting’ and now I am implanting pacemakers.
Manasa: Full circle *laughing* So we know a little about your passions outside of the workfield, and then we wanted to ask you a little bit about your dreams, beliefs, and things you want to see in the future. So what are you currently working towards in terms of your goals for things you want to happen in the next few years or the next few times past that as well.
Dr. Paydak: So one of the things I am really proud of is having this course for senior medical students that I started about 10 years ago. I myself had difficulty in learning how to read EKGs and even at the end of my one year of training in the Netherlands, my boss was confused that I couldn’t read EKGs as well as intracardiac electrograms. And then I made it a passion for myself to learn how to read EKGs which is still a learning process for me, even as a professor. But I also had this desire to teach the medical students, senior medical students, how to read them. And this is the only, I told our dean that this is the only program in the whole United States where we teach systematic reading of EKGs to our medical students, not all of them, the ones who choose my course. And unfortunately we have to limit the number to 10 a month because of limited space and etc. But my dream is to be able to teach every student that graduates from UAMS, how to read EKGs systematically and for that we have a plan with one of my fellows. We just applied for a grant to be able to start a podcast actually.
Everyone: *laughing*
Dr. Paydak: To be able to teach to all of our medical students how to read EKGs in a question answer manner. And also to be able to do some research related to this. Believe it or not, one of our senior medical students who is now becoming a resident of ophthalmology is gonna be the senior author but we do is we do pre and post test for the EKGs and then seeing, hoping that there is gonna be an improvement, we will be able to publish this and it’s gonna be the first. So my dream, personal dream, is to be able to teach at Harvard Medical School and I have had the opportunity a couple of years ago to be able to go there and work there, but I unfortunately couldn’t get the job because I wasn’t doing epicardial VP ablations or afibril ablations and etc. But that’s my personal dream. But I am very happy that we have this course and it’s my target, my hope, that we will be able to teach it to every student who graduates from UAMS. I wanna use the podcast idea and I wanna use also maybe lectures, maybe three lectures or so we will be able to add maybe two more sessions just for reading purposes. Maybe in 5-10 sessions we will be able to teach you guys.
Hannah: That sounds very helpful, as someone who we’re currently studying for step and all the outside resources, it sounds like the podcast is a wonderful idea and will be beneficial to more than just UAMS students as well. So going forward, what changes would you like to see in healthcare or what are some of your main concerns about healthcare as it is now.
Dr. Paydak: You see, I’ve been a little bit biased of being raised in Turkey, where the healthcare is provided to every citizen, like in England, like in Canada. So the other day I was thinking about this and I am still, again it doesn’t fit with the capitalist system of the United States as well, but I think it will be my desire that the biggest country in the world, the richest country in the world can provide healthcare to all of their citizens, whether they have insurance or not. But again, you know we need to educate our public that they have to abide with the rules of healthcare themselves early on, for instance in England I heard they wouldn’t do a bypass surgery to a smoker, for instance. So the public should also be educated to abide with the rules and then I think it will be better to prevent disease from happening rather than trying to clean up the things after the crash.
Hannah: As the old saying goes, prevention is the best medicine.
Dr. Paydak: Exactly
Weijia: Absolutely, so what’s one piece of advice you would give to med students in general, aside from playing chess?
Dr. Paydak: Okay the most important advice I give to anybody in life is: read the newspaper. Half an hour, it doesn’t matter what newspaper you read, it can be New York Times it can be Washington Post, it can be Arkansas Gazette, which I read every morning. But I start my day by reading the newspaper, it gives me a lot of knowledge about Little Rock, about the state, about the country, and about the world. So this is something that I have done since my childhood. My uncle used to send us newspaper everyday and the first thing anyone, my aunt is telling me that even before I knew how to read I would just go and try to read the newspaper before she read it herself. So that’s the most important advice because, especially with the interviews and everything, it will help you tremendously but I think it will also help you to become a more complete person and physician, if you know what’s going on in the city, in the state, in the country, and in the world.
Manasa: A better person as well as a more whole physician that can relate to patients better.
Dr. Paydak: Yes
Manasa: Okay so one question for you, is what is the best advice you have gotten over the years?
Dr. Paydak: I think my uncle whom I lost years ago gave me the best advice and it’s: if you are the best don’t worry about the rest.
Everyone: *laughing*
Dr. Paydak: So this is something that I’ve been trying to teach my kids as well so when they complain oh the coach played him more than I did, then I say ‘look if you’re the best you don’t need to worry about these things, just try your best at least, you can’t be the best at everything,’ as you know. But give me the best, give me your best, that’s what I’ve been trying to do everyday and that’s what keeps me going. And doing all these duties of clinical work, teaching, research, and administrative work.
Hannah: Alright, so our last little question for is a two parter it is: if you’re willing to be a mentor to students how should they best contact you or what is your preferred method of contact.
Dr. Paydak: I think that sending an email will be the easiest way because I am accessible to all the medical students and my email address is hpaydak@uams.edu. And I will be happy to meet with you for shadowing me in my clinics, attending/joining my procedures, or participating in our research projects, or in other activities you would like to get involved.
Hannah: Wonderful! Thank you so much for talking with us today. We really appreciate you taking the time out of your really busy schedule to participate in our podcast and help out our students.
Manasa: And is there anything we haven’t talked about so far that you want to make sure our listeners know about today.
Dr. Paydak: Okay I have to tell you this, I learned this from Dr. Robert Robertson, who is the head of surgery. The other day i was reading a pamphlet, again my love of reading everything and there he said ‘nothing beats experience’ ‘nothing beats experience’ so again I have had four years of EP training and I have been in this specialty for 30 years, sometimes, we have to make hundreds of decisions every day but the thing I find most helpful is my experience over the years and its something that you young students are gonna accumulate each day that you work with us and work at UAMS, but that’s something your are gonna realize when you become as mature as myself or as old as myself I should say. But that’s something that I learned from Dr. Robert Robertson and I really appreciate it.
Manasa: Well you have had a tremendous journey and we are very fortunate to have you here at UAMS.
Dr. Paydak: Thank you, thank you. Good luck to you guys during your studies and again if you choose to attend my EKG reading arrhythmias course, I look forward to working with you guys.
Hannah: Well thank you so much!
Dr. Paydak: You’re welcome!
Weijia: Thank you and listeners, if you have any comments, concerns, or suggestions, please feel free to reach out to us and let us know your thoughts!
