Initial Contact
A 12-year-old Arkadelphia girl visited the Head and Neck Oncology Clinic at the University of Arkansas for Medical Sciences (UAMS) in March after being referred by her oral surgeon. Her dentist had referred her to the surgeon after discovering, during a routine exam with X-rays, that she had a large destructive bony lesion that had eroded the entire front of her jaw.
Assessment

The lesion, believed to have been slowly growing for years, had gone undetected because the patient was relatively asymptomatic, and her parents thought the gradual protrusion of her chin was part of her normal development. Although the vast majority of lesions tend to be benign when they’re primary to the bone, as this one was, without surgery it would continue to grow, destroying additional bone, distorting the girl’s features and affecting functions like speaking and swallowing. If not addressed now, it would eventually require more extensive surgery.
Because the anterior jaw had no remaining integrity, Jumin Sunde, M.D., a head and neck surgeon, recommended a segmental mandibulectomy. This involves resecting the lesion with a clear margin, to ensure that the entire damaged area is removed. The removal of the anterior jaw would be followed by reconstructing the jaw from a vascularized section of the patient’s fibula – a non-weight bearing bone of the lower leg – in a procedure known as a free flap.
Procedures

At the patient’s second visit, Sunde and Mauricio Moreno, M.D., director of the Head and Neck Surgery Division in the UAMS College of Medicine Department of Otolaryngology, reviewed images that had been taken during the first visit. They also discussed the final surgical plan with the patient and her family. The surgery was scheduled for June 1, when the girl would be out of school.
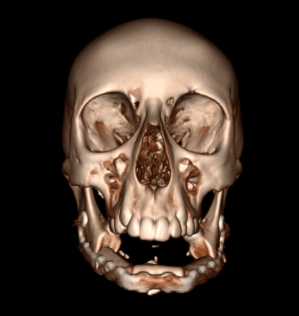
In April, Sunde and Moreno met virtually with engineers at a Colorado company to prepare for the reconstructive surgery using Virtual Surgical Planning, a tool that provides clear 3D visualization of a patient’s anatomy.
While the pre-surgical planning process was once limited to measuring, cutting and bending the pieces by hand, the virtual surgical planning technology refines the process, allowing surgeons to precisely identify the angle and location of the bony cuts in the jaw and match them to the patient’s ideal anatomy. Sunde and Moreno routinely perform fibula free flaps in the more traditional method as well when time constraints or special circumstances are less favorable for virtual planning.
The virtual sessions for adults can take as little as 10 minutes, but the situation is more complex and more time consuming when a child is involved because there are additional considerations related to the patient’s facial skeletal growth.
“It’s not removing the bone and matching what you’re removing. It’s removing the bone and matching what she’s going to grow into,” Moreno said.
The surgeons and engineers reviewed digital 3D scans of the girl’s jaw and the section of leg bone that would be used to construct a new jaw. Then the engineers made calculations to enable them to design a structural framework for the new jaw that was customized to fit the contours of the patient’s mouth.
“It’s like putting a puzzle together,” Moreno said.
Later, the engineers created templates that were shared virtually with a manufacturer in Germany, and about two weeks later, the custom-designed titanium plates arrived at UAMS.
During the surgery that followed, Moreno carefully removed the mass. Then Sunde, using the precise calculations from the virtual planning session, reconstructed the jaw by inserting the fibula free flap, cut into three pieces to accommodate the curvature of the jaw, side-by-side inside the structural titanium framework.
Within several months, the three segments will have naturally fused together by a stable bony union similar to how a fracture heals.
“We expect to see full fusion between those segments in the native jaw,” Moreno said. “It all becomes one single piece of bone.”
The new jaw was designed so that the patient can grow into it as she reaches skeletal maturity, typically at about 17 years of age.
Follow Up

The patient was walking the day after surgery. Days later, the only obvious sign of her surgery was a single linear scar down her leg and a curved neck incision hidden in natural skin creases.
She was discharged to home five days after surgery, on June 6. She was placed on a diet limited to soft foods to prevent her from chewing and to give the new jaw time to set and heal at her first post-operative follow up two weeks after surgery.
Because the removal of the anterior jaw also involved removal of some of the patient’s teeth, she will receive dental implants in four to six months.
At her second post-operative visit six weeks after surgery, she has resumed normal activities and is tolerating a soft diet without any difficulty. A CT scan shows that her new jaw is already well along in healing.
Discussion
Sunde said the lateral lower leg bone is often used in jaw reconstructions because it has significant bone stock that can support dental implants. Because it is located in a non-weight bearing section of the leg, it doesn’t generally affect a patient’s use of the leg unless the patient participates in certain sports involving fast turns that require extra ankle stabilization.
The expertise and experience provided by Moreno and Sunde has enabled UAMS to perform more than 55 free flap surgeries using virtual planning in the past three years – far more than any other institution or surgical group in the state.
Both doctors are fellowship-trained and are part of UAMS’ Head and Neck Surgery team, which treats head and neck cancers, benign tumors, traumatic injuries and other conditions.
The team members also contribute to research and surgical innovation on an international scale. They treat squamous cell carcinoma, thyroid cancer, parathyroid tumors, vascular malformations, salivary gland tumors, skull base tumors, traumatic injuries and other complex issues involving the head and neck.
The department is a national and international leader, and its ear, nose and throat services are ranked among the top 50 in the nation by U.S. News and World Report.
To make a referral to the UAMS Head and Neck Cancer Clinic at the Winthrop P. Rockefeller Cancer Institute in Little Rock, call 501-296-1200.
Biographies
Mauricio Moreno, M.D.
Associate Professor
Department of Otolaryngology – Head and Neck Surgery
Doctor of Medicine, Pontificia Universidad Catolica de Chile School of Medicine in Santiago, Chile
General surgery, University of Valparaiso in Chile
Otolaryngology Head and Neck Surgery, University of Chile in Santiago, Chile
Head and Neck Surgical Oncology, Microvascular Reconstructive Surgery and Surgical Endocrinology, all at the University of Texas M.D. Anderson Cancer Center, Houston, Texas
Jumin Sunde, M.D.
Assistant Professor
Department of Otolaryngology – Head and Neck Surgery
Doctor of Medicine, University of Alabama at Birmingham School of Medicine
Head and Neck Surgery, UAMS
Head and Neck Surgery, UAMS
Microvascular surgery, University of Michigan