Hidradenitis suppurativa (HS) is a skin disorder that starts with blocked hair follicles, leading to painful nodules, abscesses and scarring. Front-line providers can work with dermatologists to diagnose and treat this often debilitating condition by asking three questions and following a five-tiered approach to treatment.
Dr. Vivian Shi, former UAMS dermatologist and director of the hidradenitis suppurativa clinic, offered tips to family medicine providers at the UAMS 2024 Family Medicine Spring Review last April. She said, “It requires a multidisciplinary approach. An HS team including all of these specialists and dermatology providers are the principal providers, but we really lean on front-line providers … to detect, treat, refer and to collaboratively manage.”

Most of her HS patients have had it more than 10 years after having seen their providers at least five times, and around 15% are disabled or unable to work because of HS pain. Girls typically show signs in their early teens, and boys start in their mid to late teens. If the teen has severe acne, have the patient lift the arms to check for HS signs. The typical onset is between puberty and age 40, with women being three times more likely to be affected.
Three key diagnostic questions every provider must ask the patient:
1. In the last 12 months, did you repeatedly have big, painful nodules and boils in the armpits or groin?
2. Have you had outbreaks of boils in the last six months?
3. Do you repeatedly have outbreaks of big sores, painful nodules or boils that heal with scars in any of these locations?
If the answer is “yes,” there is a 90 percent chance of HS.
“There’s no reason healthcare providers should be missing this if they ask these questions,” said Dr. Shi.
HS can show up anywhere on the body – behind the ears, outer arms or legs – not just the skin folds and areas with sweat glands. The two exceptions are the palms and soles of the feet. It’s chronic, inflammatory and very painful. Initially, the patient will have inflamed nodules, abscesses, white heads and black heads. The more advanced stage includes draining sinus tracts (narrow channels) and severe scarring, which are especially true in Blacks. Often it is misdiagnosed as cellulitis.
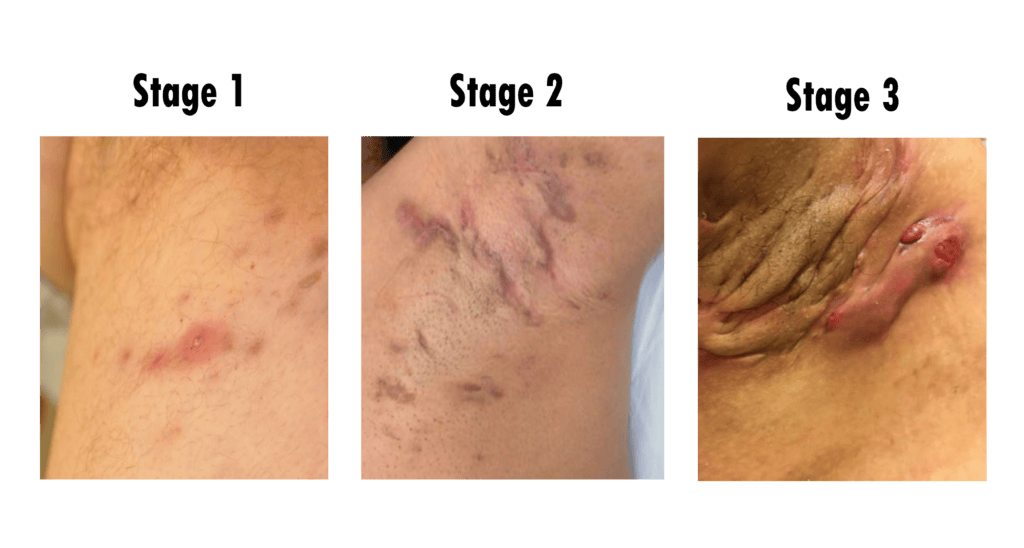
HS is divided into three Hurley Stages. The mildest is Hurley Stage 1: Abscesses that resolve without any trace of scarring, but this is rare. As soon as the patient has any sign of a scar, it’s labeled Hurley Stage 2. This stage includes recurrent abscesses, sinus tracts and scarring, but normal-looking skin will appear between them. The most advanced stage is Hurley 3, characterized by multiple connected sinus tracts and abscesses across the entire area with little to no normal-looking skin between. She describes it as an “over-exaggerated inflammatory response where, over time, the hair follicles connect with each other and form sinus tracts and extensive scarring.”
Dr. Shi recommended a pyramid of treatment. The front-line provider can manage all the treatments except for biologics, the top tier. In early moderate to severe patients (late Hurley 1 to early Hurley 2), Dr. Shi suggested preparing patients for biologic therapy by prescribing oral antibiotics because payors typically require patients to fail 90-plus days of systemic antibiotics to qualify. Regardless of disease stage, providers should refer the patient to a dermatologist for advanced therapy, while collaboratively managing the patient.
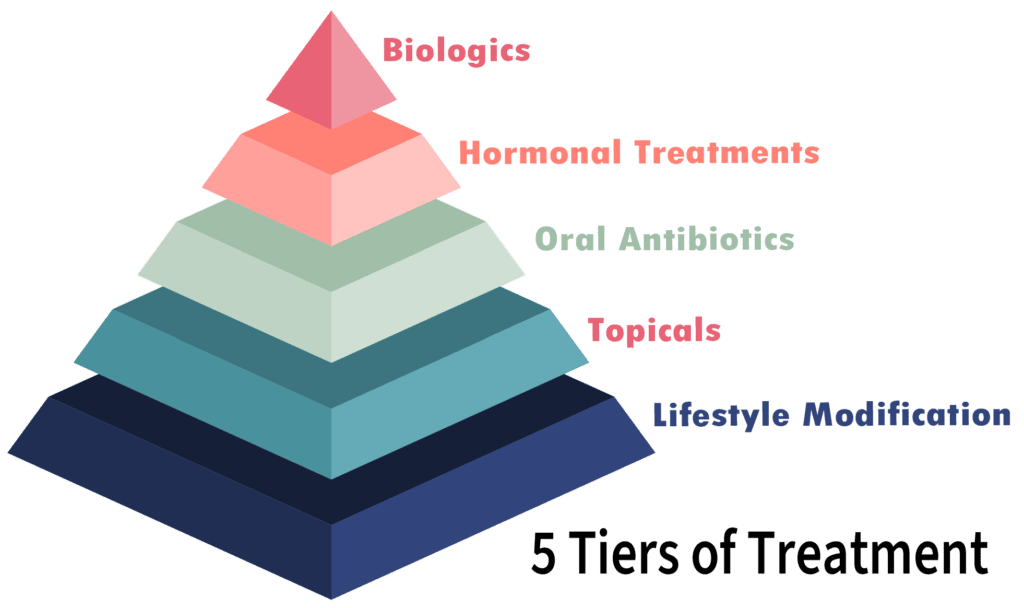
Lifestyle Modification
The first tier of the pyramid is lifestyle modifications where the provider would screen for comorbidities and start treatments. In a recent JAMA Dermatology report, patients with HS said diet changes were the most used non-prescription treatment with the Mediterranean diet and intermittent fasting both being effective. The two exercises that HS patients can tolerate are Pilates and swimming. Weight loss surgery is also a strong consideration if the patient is greater than 35 BMI, and if the patient smokes, encourage them to quit since cigarette smoke has dioxin-like compounds that can cause acne and scarring. Loose-fitting clothing and anti-chaffing products applied in skin folds can reduce friction and pain.
If the patient has draining sinus tracts, bathing helps to rinse out the tunnels. Dr. Shi recommends alternating daily with 10-minute baths of Epsom salt, CBD oil and ¼ cup 6% commercial bleach which help with pain, itch, relaxation and decrease biofilm.
Topicals
The next level is topical treatments. She typically uses clindamycin 1%; however, resorcinol 15% elicits a better response in mild to moderate HS. Resorcinol is especially helpful because it breaks down the outer layers of the skin and unplugs the hair follicles. There are also washes such as benzoyl peroxide, chlorhexidine or dapsone. Dr. Shi cautioned against benzoyl peroxide wash used together with topical dapsone because they’ll have reversible yellowing of the hair follicles.
Oral Antibiotics
Dr. Shi’s office typically starts with the tetracycline family because it’s better at reducing inflammation in the hair follicle and less costly. She recommends 100 milligrams of doxycycline or minocycline twice daily or extended release minocycline at a weight-adjusted dose once a day for eight to 12 weeks. Dr. Shi cautioned that dosage may need to exceed 100 milligrams for it to work, so ensure the patient doesn’t have anemia. She uses this for flare-ups or to bridge to biologic therapy.
Rotating through combined systemic antibiotics also works, being careful not to extend beyond three months. One combination is clindamycin with rifampin. A second choice is rifampin with moxifloxacin and metronidazole, which is especially helpful for drainage. And one thing providers want to consider is to stop the metronidazole after six weeks because longer use can cause reversible peripheral neuropathy.
Certain supplements also should be considered. Persons with HS typically have lower serum zinc levels. Prescribing 100 – 200 milligrams of daily zinc (with copper included after two months) has shown to reduce HS severity in 80% of patients. Another supplement to consider is Vitamin D since most patients with HS are deficient. Vitamin D regulates hair cycle and skin cell activity.
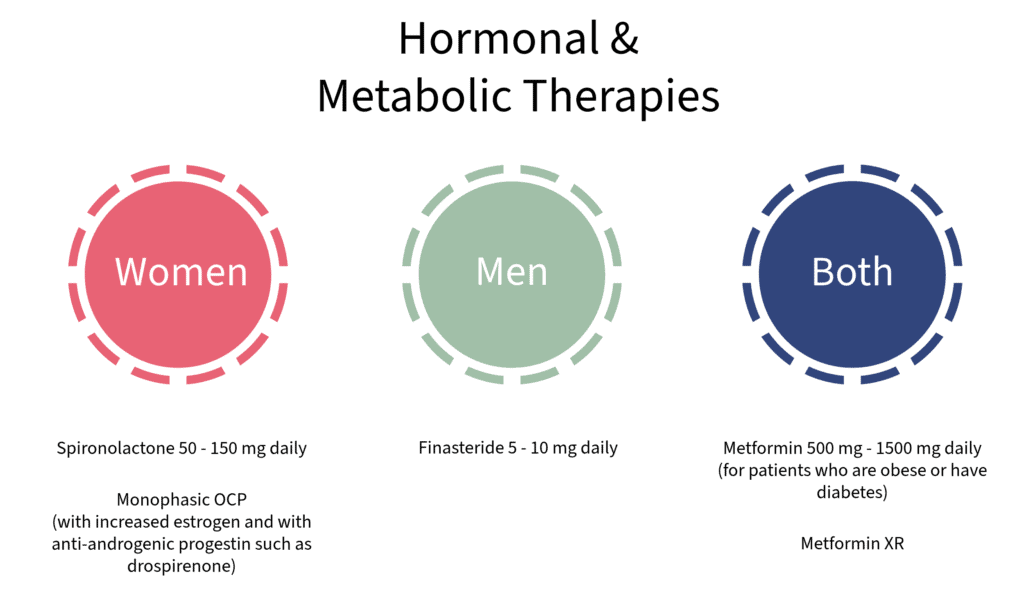
Hormonal Treatments
Dr. Shi recommends these hormonal / metabolic therapies:
Biologics
Biologics is the last step of treatment. Dr. Shi said providers should learn the basics of biologics so they can explain how it works before they refer to a dermatologist. The patient must be on at least 90 days of an oral antibiotic before most insurance will allow biologics.
Dr. Shi’s takeaways:
- Ask the three questions to have a high confidence of diagnosing HS.
- Refer to dermatology once diagnosed.
- Screen for metabolic syndromes, inflammatory bowel disease, hormonal and mental health abnormalities.
- Reverse screen for HS if the patient has Down syndrome.
- Start antibiotics if the patient has any scarring because biologics is the next step. Most insurance requires 90 days to four months of oral antibiotic to be eligible for biologic treatment, so this is the referral window.
- More information on HS can be found at hs-foundation.org
If you’re interested in more of UAMS’ primary care CME/CE, check out our list of upcoming CME/CE here.