Irritable Hip
What is it?
A very common sighting in any pediatric emergency department is the child who presents with refusal to bear weight, sudden limp or atypical irritability and crankiness. In this setting, the differential can vary from relatively harmless conditions like transient synovitis to life threatening septic arthritis, which is the most dreaded possibility requiring a swift diagnosis to avoid destruction of the articular cartilage and reduce the risk of developing early arthritis.
Septic arthritis, a surgical emergency, is always to be suspected when a child of any age presents with hip pain, fever, irritability and toxic appearance without a history of trauma. Elevated white count and inflammatory markers (ESR and CRP) and decreased range of motion at the hip (presumably due to inflammatory fluid in the joint space) may help point towards this diagnosis as well (1). Toxic synovitis is the diagnosis with the highest incidence rate (6) but remains a diagnosis of exclusion.
Toxic synovitis, which is also known as transient synovitis for its transient aseptic inflammatory nature is a much milder infection and is presumed to be a post viral syndrome of sorts. Generally, these children exhibit no significant pain on palpation and do not present with marked limping
How does it happen?
Most cases of septic arthritis occur from direct extension of bacterial infection (Staphylococcus aureus is frequently the causative organism) from the adjacent metaphysis (2).
What do I need to know?
Diagnostic evaluation frequently begins with hip joint radiographs which may be unrevealing or may show widening of the joint space, which is a nonspecific finding (4). Ultrasound is widely cited as the gold standard (5) for the assessment of the presence and extent of joint effusion as the absence of joint effusions effectively eliminates septic arthritis (3, 4). Joint effusion negative for organisms on aspiration and WBC count (<20k) are markers of bland inflammatory joint fluid not requiring surgical management.

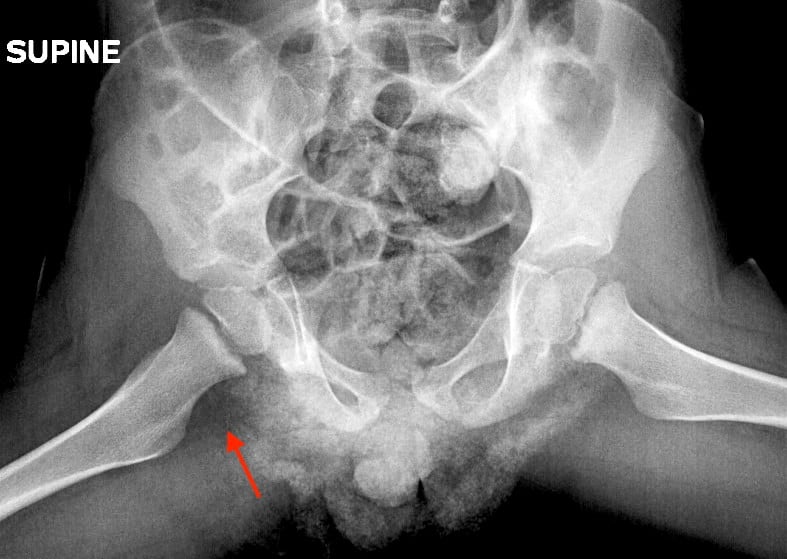
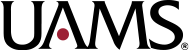
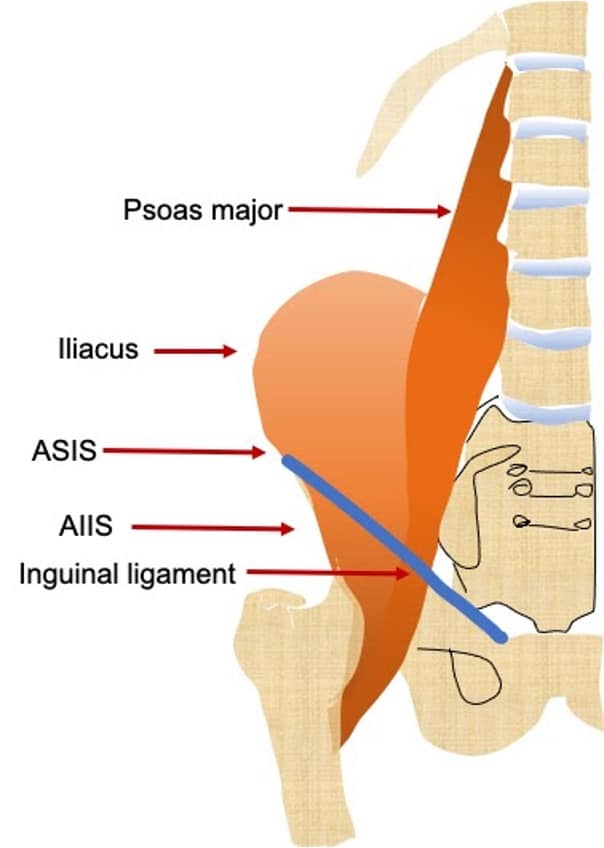
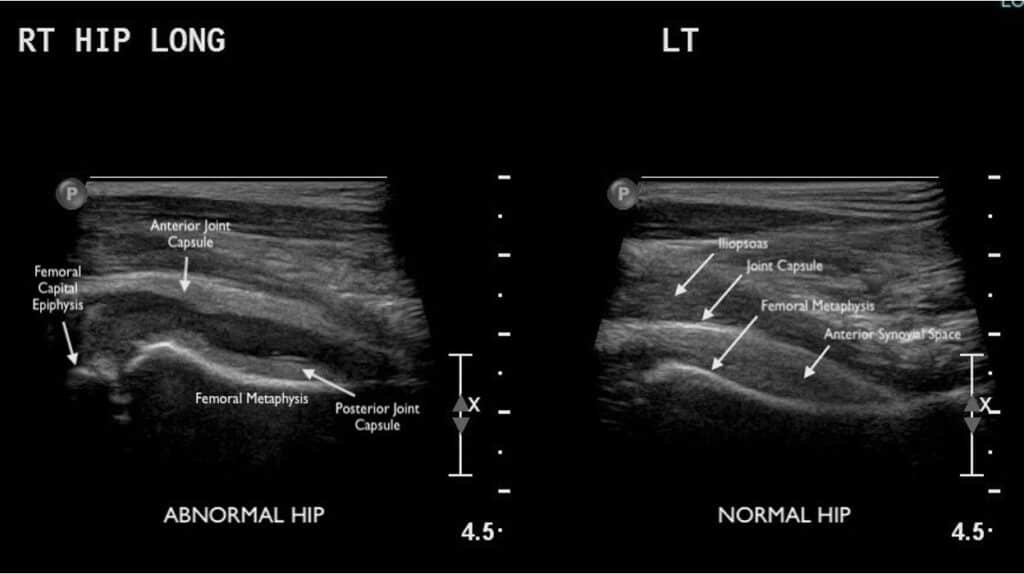
Ultrasound of both the affected and unaffected hip joints can be performed in the parasagittal approach for comparison and documentation purposes. The hip joint is a synovial joint formed by the femoral head and acetabulum and is enclosed by the fibrous capsule. The anatomical landmarks of the hip joint are demonstrated the final image. To look for hip effusion, measure the distance between the anterior surface of the femoral neck and the posterior surface of the iliopsoas muscle coursing anteriorly to the hip joint (see figure). Normally, there is some fluid within the joint capsule (<5 mm) but sonographic criteria for a pediatric hip joint effusion are:
- Fluid collection greater than 5 mm
OR
- Asymmetrical joint difference of >2 mm when compared to the contralateral side (1, 7)
If there is an effusion on ultrasound, US guided aspiration is generally the next step to differentiate between the more critical septic arthritis and the more indolent transient synovitis. As no sonographic signs can be used to differentiate a sterile from a purulent or hemorrhagic exudate (8). So a simple rule of thumb is, if you see fluid in a joint, it needs to be tapped.

What do I need to do?
Promptly notify the IR attending on call to expedite management as time is of the essence. In the IR suite, informed consent is obtained and conscious sedation is employed before rescanning the patient in the anterior parasagittal plane and determining the angle of approach. The site is then prepped and draped, local anesthesia is instilled and a small skin incision is made to guide a 20-gauge spinal needle through the skin. Ultrasound transducer probe covered by a sterile sheath and sterile acoustic gel is utilized to localize the site and through sonographic real time monitoring, the needle is guided into the joint space and aspiration of the fluid is attempted. If no fluid is obtained and the needle was sonographically evident to have been in the joint space, a larger gauge needle is used to aspirate the viscous synovial fluid. The fluid is then sent for cell count, culture and Gram stain. Determination of operative management is based on the WBC count (>50k) and positive Gram stain and culture.
Selected References:
1. Zawin, J. K., Hoffer, F. A., Rand, F. F., & Teele, R. L. (1993). Joint Effusion in Children with an Irritable Hip: US Diagnosis and Aspiration. In Radiology (Vol. 187).
2. Ciambotti, J., Lai, W., Cook, C., Altes, T., Casey, E., Pirttima, T., Pirttima, S., Mentore, K., HIgginbotham, J., Gupta, A., Mcllhenny, J. and Gay, S., 2020. Septic Arthritis And Toxic Synovitis. [online] Med Ed Virginia. Available at: <https://www.med-ed.virginia.edu/courses/rad/peds/ms_webpages/ms3dseptic.html> [Accessed 8 August 2020].
3. Pade, K., Lobo, V. and Gharahbaghian, L., 2020. Tips & Tricks: Ultrasound In The Diagnosis Of A Pediatric Hip Effusion. [online] Acep.org. Available at: <https://www.acep.org/how-we-serve/sections/emergency-ultrasound/news/april-2018/tips–tricks-ultrasound-in-the-diagnosis-of-a-pediatric-hip-effusion/> [Accessed 8 August 2020].
4. Bomer, J. and Holscher, H., 2020. The Radiology Assistant: Hip Pathology In Children. [online] Radiologyassistant.nl. Available at: <https://radiologyassistant.nl/pediatrics/hip/hip-pathology-in-children> [Accessed 8 August 2020].
5. Wright, N., & Choudhery, V. (2000). Diagnostic imaging of the hip in the limping child. In Journal of Accident and Emergency Medicine (Vol. 17, Issue 1, p. 48). BMJ Publishing Group. https://doi.org/10.1136/emj.17.1.48
6. Krul, M., Van Der Wouden, J. C., Schellevis, G., Van Suijlekom-Smit, L. W. A., & Koes, B. W. (2010). Acute non-traumatic hip pathology in children: incidence and presentation in family practice. Family Practice, 27, 166–170. https://doi.org/10.1093/fampra/cmp092
7. Vieira, R. L., & Levy, J. A. (2010). Bedside Ultrasonography to Identify Hip Effusions in Pediatric Patients. Annals of Emergency Medicine, 55(3), 284–289. https://doi.org/10.1016/j.annemergmed.2009.06.527
8. Tay, G., Ashik, M., Tow, B., & BL Lim, K. (2013). Hip Pain in The Paediatric Age Group – Transient Synovitis Versus Septic Arthritis. Malaysian Orthopaedic Journal, 7(2), 27–28. https://doi.org/10.5704/moj.1307.011