Testicular Torsion
What is it?
Twisting of the testis, presenting as acute scrotal pain, redness and swelling in children (commonly bimodal (1) among newborns and teenagers) with or generally, without trauma.
How does it happen?
Testicular torsion occurs when the testis twists around its axis, i.e. the spermatic cord causing obstruction of venous flow → engorgement of the testicle → edema and swelling → rising parenchymal pressures → arterial inflow obstruction → eventually, necrosis and infarction of the germinal tissue. This process can be stopped within <6 hours of presentation to avoid frank tissue death and loss of testis.
What do I need to know?
Although not the most common cause of severe acute scrotal pain in children and superseded by torsion of the testicular appendix and epididymitis in incidence (2), it is crucial to exclude torsion of the testes as a cause of acute scrotum for timely management of this critical condition.
Remember, reading a possible torsion case should be HIGH priority.
Use of a high frequency linear transducer (7-13) MHz and Color and Spectral Doppler (triplex Doppler) are essential for accurate diagnosis. Start from the normal side and move to the abnormal side. Make sure the ‘buddy view’ is included in the series so you can compare both testes side by side.
Key ultrasound features to look for in testicular torsion:
- Note the echotexture of the testicular parenchyma – which is normally homogenous, an infarcted testicle may appear inhomogenous, hypoechoic compared to the normal side and may be accompanied by a reactive hydrocele (features which denote irreversible damage and low likelihood of surgical salvage
- Note the size – the affected side may be larger and edematous with/without overlying scrotal wall thickening
- Color Doppler – complete absence of intratesticular blood flow vis a vis normal blood flow on the unaffected side is diagnostic of torsion although commonly not observed – note presence/absence of central perfusion as often peripheral perfusion may be preserved
- Spectral Doppler features:
- Look for antegrade and patent venous waveforms – early sign of torsion
- Measure resistive indices (RI) of the testicular vessels
- Concept – testicular germinal epithelium is metabolically active in the post pubertal stage and therefore has lower resistive indices with antegrade diastolic flow
- >0.7 or reversal of flow may indicate partial torsion
- For prepubertal children, RI values up to 1 are considered normal (3)
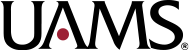
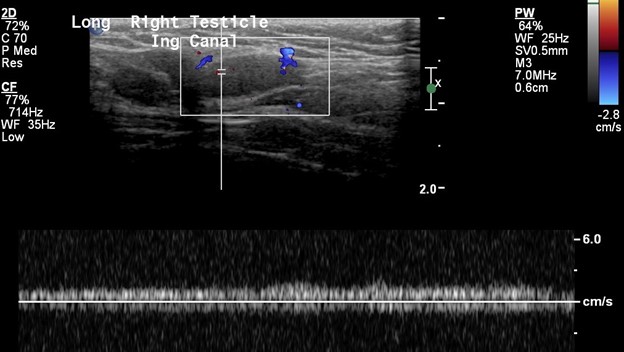
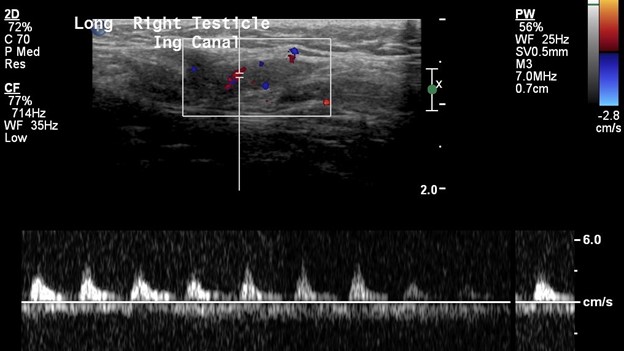
Note the normal size and shape of the right testicle which demonstrates normal color flow. The spectral waveforms are well maintained.

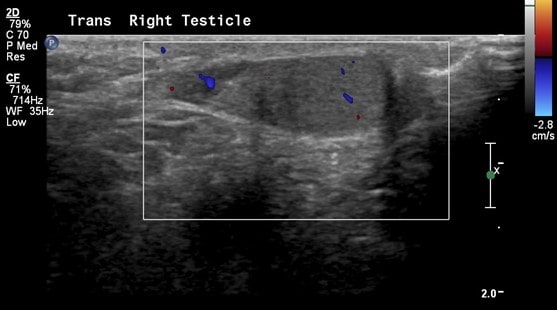
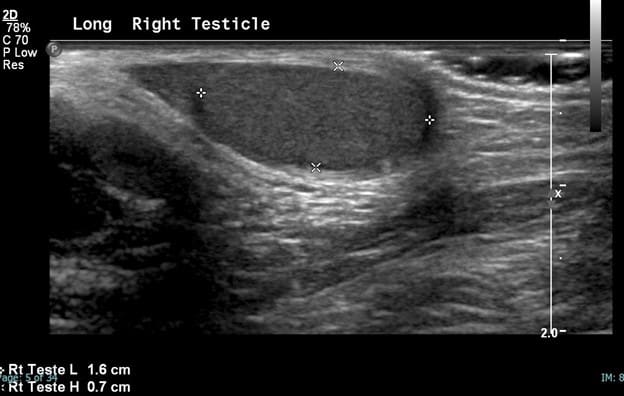

The right epididymis is also normal in size, shape and echotexture with preserved flow on color Doppler.
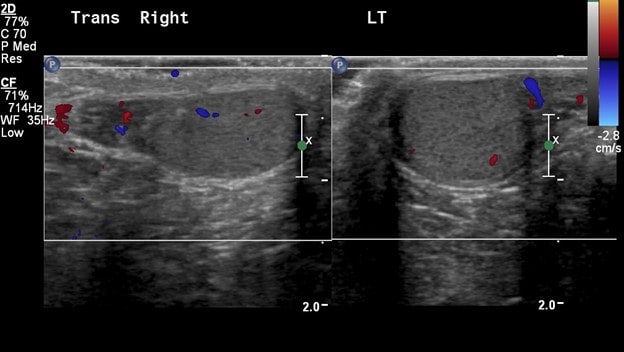
The left testicle is homogeneous, symmetric in size and shape and demonstrates preserved color and Doppler waveforms.



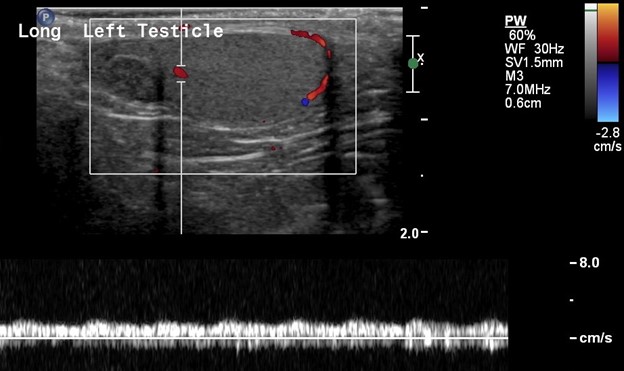
Remember, presence of arterial perfusion does not exclude partial torsion.
Sometimes, the torsion is intermittent and can undergo spontaneous detorsion (2) which can impede definite sonographic diagnosis at the time of scan.
Important clinical mimics of testicular torsion to be aware of include torsion of the appendix testis and epididymo-orchitis because they present similarly with acute scrotal pain but can be reliably and confidently diagnosed on imaging.
When instead of the testis, the small appendages associated with the testis and epididymis undergo torsion and become ischemic, the diagnosis is that of testicular appendix torsion. These appendages are embryological remnants of the Wolffian and Mullerian ducts (3) and lie directly above the testis. Typically, these patients present with more insidious pain.
The left epididymis is normal; however, just beside the epididymis lies an ovoid, heterogeneously hypoechoic structure measuring 0.5 x 0.4 cm which demonstrates no flow on color Doppler representing a torsed, and infarcted testicular appendage.


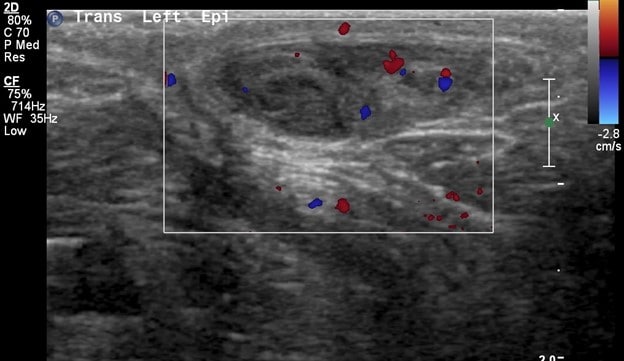
Sonographic features of testicular appendix torsion:
- Hyperechoic/hypoechoic, round structure medially located next to the upper pole of the testis between the epididymis and testis
- Heterogeneous echotexture with poor or no perfusion on color Doppler
- No definite size criteria, however literature suggests cut off of >5.6 mm (4) for 100% specificity
- Often associated with enlargement and reactive hyperemia in the epididymis (likely reactive) (3)
It is important to distinguish appendix torsion from frank testicular torsion because the treatment for appendix torsion is generally symptomatic while torsion of the testis is a true surgical emergency.
Epididymo-orchitis has relatively classic imaging features and may be associated with dysuria due to concomitant urinary tract infection. Look for an enlarged, hyperemic epididymis with low RI values (3) with similar inflammatory changes in the testis on the affected side.
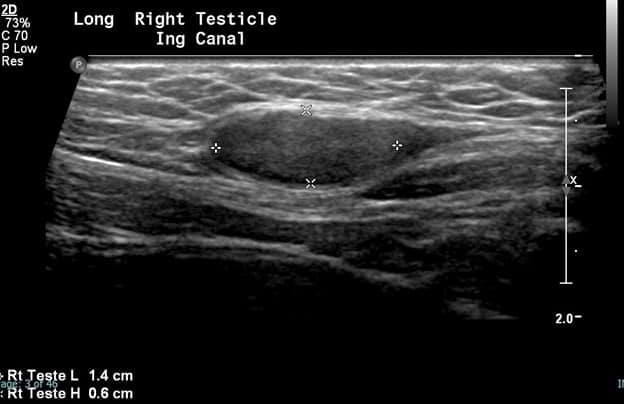
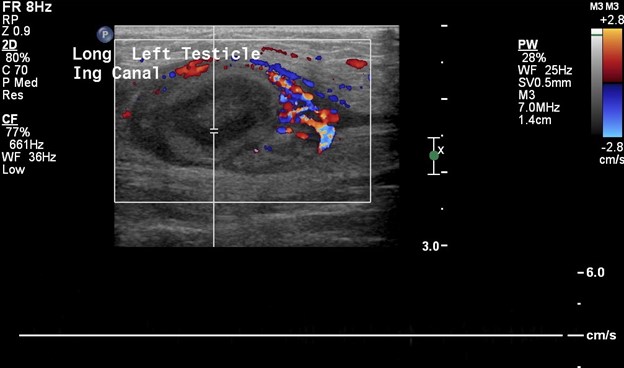
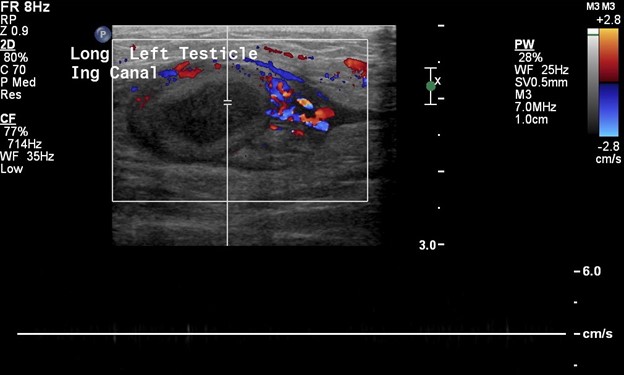
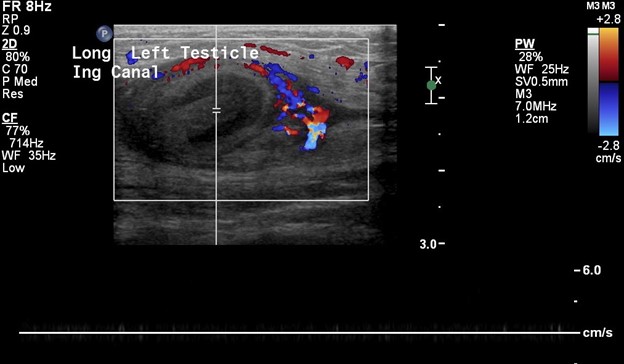
In this patient, the right testicle lies within the inguinal canal but demonstrates a homogeneous echotexture with preserved color and spectral Doppler waveforms as well as a normal size and shape. The right epididymis also lies within the inguinal canal but is normal in morphology.



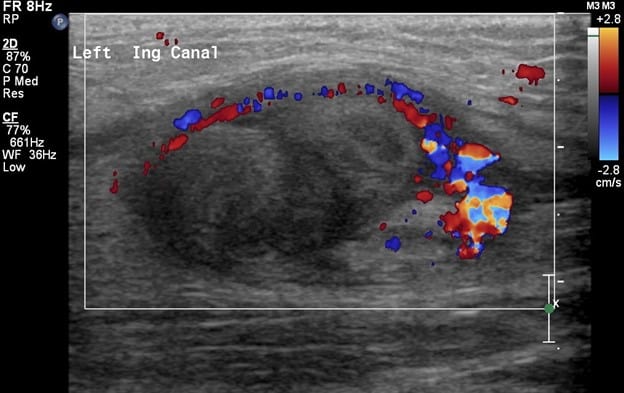
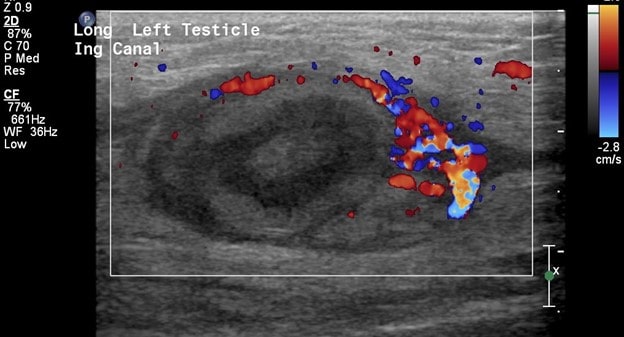
In comparison, the contralateral inguinal canal contains an enlarged oval structure with extremely heterogeneous echotexture and significantly increased peripheral flow on color Doppler. The longitudinal ultrasound of the inguinal canal demonstrates the increased size to best advantage. Note no flow on color/spectral Doppler. On the second to last image, the power Doppler is being utilized to show absent flow within the testicle. The last image shows a normal left epididymis. Findings are in keeping with an infarcted left inguinal testes.






Selected Resources:
- Govindarajan, K., Nelson, C., Windle, M., & Cendron, M. (2020). Pediatric Testicular Torsion: Background, Anatomy, Pathophysiology. Retrieved 5 September 2020, from https://emedicine.medscape.com/article/2035074-overview#a6
- Lonergan, G. (2020). The Radiology Assistant : Acute Scrotum in Children. Retrieved 5 September 2020, from https://radiologyassistant.nl/pediatrics/acute-scrotum/acute-scrotum-in-children
- Günther, P., & Rübben, I. (2012). The Acute Scrotum in Childhood and Adolescence. Deutsches Arzteblatt International, 109(25), 449–458. https://doi.org/10.3238/arztebl.2012.0449
- Baldisserotto, M., de Souza, J. C. K., Pertence, A. P., & Dora, M. D. (2005). Color Doppler Sonography of Normal and Torsed Testicular Appendages in Children. American Journal of Roentgenology, 184(4), 1287–1292. https://doi.org/10.2214/ajr.184.4.01841287