Cranial Ultrasound
Cranial ultrasonography remains an important tool to evaluate for hydrocephalus, periventricular leukomalacia (PVL, also known as hypoxic-ischemic encephalopathy of the preterm) and intracranial hemorrhage.
The most common reason for cranial ultrasound is to look for bleeds. In a premature baby, germinal matrix hemorrhage, screening for intracranial hemorrhage before the newborn is placed on Extracorporeal Membrane Oxygenation (ECMO) and during ECMO (for which the patient will be heparinized), also rarely to look for bleeding as source of seizure/apnea in infants.
Why are cranial ultrasounds the modality of choice for evaluation of cranial abnormalities in the neonate?
Advantages include portability, accessibility, lack of ionizing radiation, no need for sedation and the ability to perform baseline and serial scans for comparison.
How do we perform a cranial ultrasound?
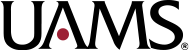
Scans are performed through an open acoustic window (typically the larger anterior fontanelle) with the addition of other acoustic windows as required for assessment (posterior/lambdoid fontanelle, squamosal part of temporal bone/temporal window, mastoid fontanelle, coronal and squamosal sutures, etc) usually with a 7.5-8 MHz transducer (9, 10).
Neurosonography is performed through the coronal and sagittal planes. Multiple static images are taken to demonstrate the frontal lobes, corpus callosum, lateral ventricles, basal ganglia structures and occipital lobe in the coronal projection. The interhemispheric fissure demarcates the mid-sagittal plane where the junction of the thalamus and caudate (caudothalamic groove) can be best appreciated. This is important because it is the most common site of germinal matrix hemorrhage. Parasagittal images are also obtained to visualize the peripheral aspects of the ventricles and bilateral cerebrum (9, 10).
What are some helpful interpretation concepts for translating normal cranial anatomy on ultrasound?
- Gray matter appears hypoechoic while white matter is hyperechoic due to fatty myelin.
- Reversal of this pattern indicates an underlying abnormality.
- Normal brain is always symmetric although it is important to note that symmetry is not always normal. It is important to recognize bilateral symmetric abnormalities (8).
- Normal echogenicity of the white matter surrounding the ventricles (periventricular white matter – PWM) is lower than the echogenicity of the choroid plexus. PWM is also homogeneous in appearance. Reversal of this pattern indicates PVL which can predispose to the development of cerebral palsy (7, 8).
- Look for the superficial pia mater which is seen as a thin, echogenic layer immediately overlying the hypoechoic cortex, which lies above the hyperechoic white matter (8, 9).
What are the important structures to identify in a cranial ultrasound?
- Lateral ventricles – to look for hydrocephalus
- Corpus callosum – to look for agenesis, anatomical variants of the septum pellucidum (cavum septum pellucidum, cavum vergae, cavum velum interpositum)
- Periventricular white matter – to look for PVL
- Caudothalamic groove – to look for grade 1 germinal matrix hemorrhage
- Choroid plexus – to look for choroid plexus hemorrhage (more common in term infants)

What is the germinal matrix?
The germinal matrix is a cellular, highly vascular site where neuroblasts originate. It is located in the subependymal region of the lateral ventricles at the caudothalamic groove and contains fragile blood vessels that are prone to rupture with variations in neonatal stresses. The germinal matrix completely involutes by 36 weeks of gestation and therefore germinal matrix hemorrhages are rare in term neonates.
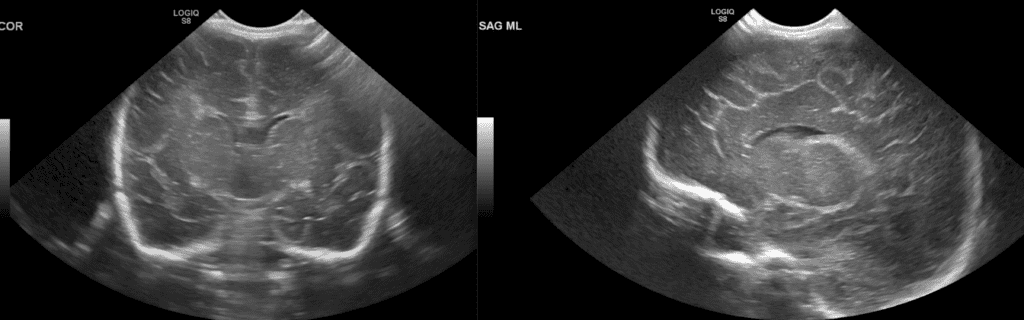
Since the germinal matrix resides in the caudothalamic groove, germinal matrix hemorrhage appears as an echogenic ovoid structure within the caudothalamic groove. The common confounder is the choroid plexus which is also bright on ultrasound and is a normal part of the lateral ventricles.
So how do I tell them apart?
You can distinguish between the normal choroid plexus and germinal matrix hemorrhage on a parasagittal ultrasound image by paying attention to the anterior extension of the echogenicity. Normal choroid never extends as anterior as the caudothalamic groove on an off midline sagittal view (11). Clear as mud?
How to grade germinal matrix hemorrhages?
Grade I – confined to the caudothalamic groove (most common)
Grade II – extends into the lateral ventricles but there is no hydrocephalus

Grade III – extends into the lateral ventricles and there is hydrocephalus

Grade IV – intraparenchymal hemorrhage (highest mortality). Hypothesized to be due to venous infarction vs direct extension of intraventricular hemorrhage (11)

Selected References
- Beek, E., & Groenendaal, F. (2020). The Radiology Assistant : Neonatal Brain US. Retrieved 13 September 2020, from https://radiologyassistant.nl/pediatrics/neonatal-brain-us/neonatal-brain-us
- Lowe, L. H., & Bailey, Z. (2011). State-of-the-art cranial sonography: Part 1, Modern techniques and image interpretation. American Journal of Roentgenology, 196(5), 1028–1033. https://doi.org/10.2214/AJR.10.6160
- Bhat, V., & Bhat, V. (2014). Neonatal neurosonography: A pictorial essay. Indian Journal of Radiology and Imaging, 24(4), 389–400. https://doi.org/10.4103/0971-3026.143901
- Gupta, P., Sodhi, K. S., Saxena, A. K., Khandelwal, N., & Singhi, P. (2016). Neonatal cranial sonography: A concise review for clinicians. In Journal of Pediatric Neurosciences (Vol. 11, Issue 1, pp. 7–13). Medknow Publications. https://doi.org/10.4103/1817-1745.181261
- Donnelly, L. F. (2009). Pediatric Imaging: The Fundamentals. United Kingdom: Saunders/Elsevier.