Intussusception
What is it?
Intussusception is the most common cause of intestinal obstruction affecting the 6-and 36-months age group, with the majority (80-90%) of intussusception cases affecting children <2 years of age with maximal incidence just under 12 months (1, 7). Although abdominal pain is usually the most reliable clinical symptom in older children above the age of 1 year presenting with acute intussusception, emesis, irritability and bloody stooling (currant jelly stools) are the strongest clinical predictors in children younger than the age of 12 months (7).
How does it happen?
Intussusception is conceptually simple to understand, as it refers to invagination or telescoping of one bowel segment into another, with the proximal segment being referred to as the intussusceptum and the distal segment as the intussuscipiens (the segment that contains/receives the invaginated bowel). As the condition develops, the mesentery surrounding the intussusceptum is dragged along with it into the distal segment causing lymphatic and venous congestion, leading to intestinal edema and eventual vascular compromise resulting in ischemia, necrosis, perforation and peritonitis.
What do I need to know?
Ultrasound is the preferred modality with a specificity of 100% (2).
Sonographic diagnosis of intussusception is relatively straightforward with the following findings:-
- Transverse plane: Classic “target” or “doughnut” appearance – Hypoechoic outer layer indicating edematous bowel
- Longitudinal plane: “Pseudokidney” appearance – Greater than 3 cm in dimension.
An important differential to consider when evaluating ultrasound findings of intussusception is small bowel – small bowel intussusception and distinguishing it from ileocolic intussusception which is a true surgical emergency. Small bowel – small bowel intussusception is smaller, self-limiting and usually disappears during the exam or shortly afterwards (the tech can rescan the patient after a little while to make sure the intussusception disappears).
Also note that if you see lymph notes inside the intussusception, hyper echoic core on ultrasound (this represents mesenteric fat), or when you can’t see a normal ileocecal (IC) junction sonographically, your suspicions for ileocolic intussusception should be strongly heightened.
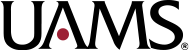
Axial contrast enhanced CT at the level of the common iliac arteries. Cine loop demonstrates “bowel within bowel” appearance with the outer layer representing the intussuscipiens (cecum) and the inner layer representing intussusceptum (distal ileum).
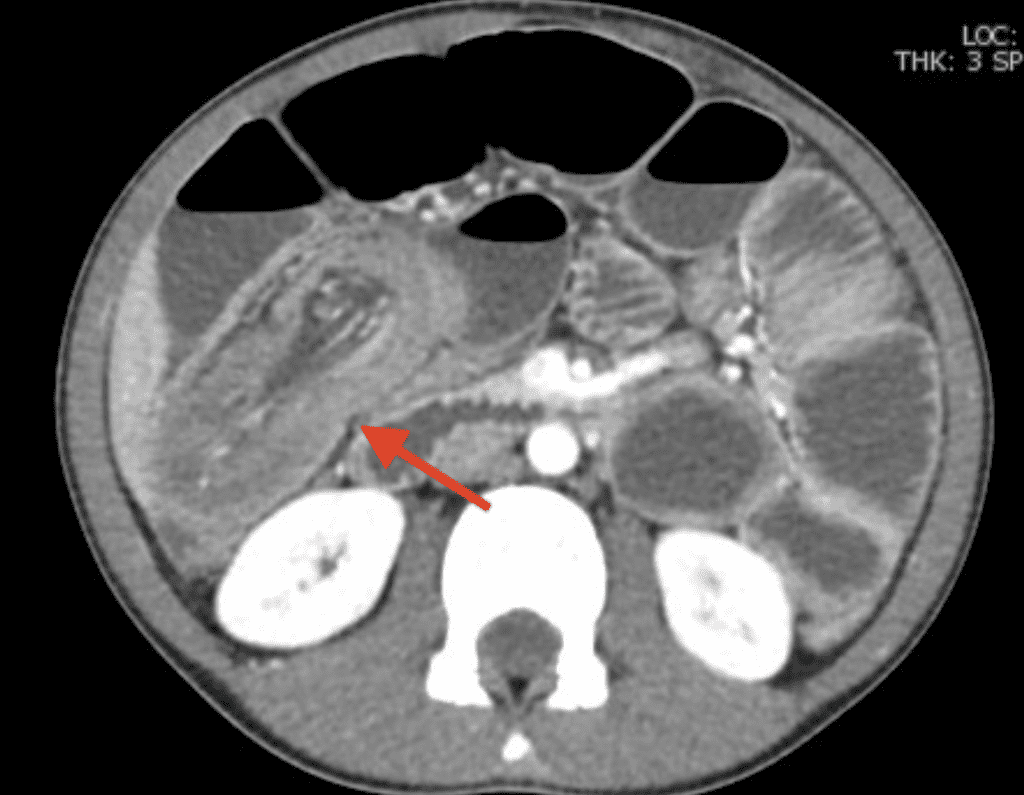
Beautiful example of ileocolic intussusception is demonstrated in this coronal contrast enhanced MIP CT stack. Note long segment intussusception of the terminal ileum throughout the entire length of the cecum up to the ascending colon in the right upper quadrant.


Note there is little to no bowel wall perfusion, this is extremely worrisome. Absence of bowel wall perfusion is more concerning than hyperemia. You also have to look for presence of ascites on US – another alarming sign.
Cine grayscale longitudinal ultrasound image of the right lower quadrant. “Pseudo kidney” sign: Note kidney-like appearance with multiple thin, parallel hypoechoic and echogenic stripes.
What do I need to do?
For the radiology resident on call, the diagnosis of small bowel – large bowel intussusception could potentially be just the beginning of events, as the best treatment for most patients with normal vital signs involves non operative reduction with hydrostatic or pneumostatic pressure under fluoroscopy. The next steps would entail calling the techs to help set up the fluoroscopy suite, arranging to stabilize the patient on intravenous fluids if volume depleted and starting the patient on intravenous antibiotics (dependent on institutional policy) and lastly and most importantly, calling in the on-call Pediatric Radiologist and the surgery team who will be standing by during the procedure in case the enema reduction fails or perforation occurs.In our institution, we usually perform a pneumatic fluoroscopically guided intussusception reduction as follows:
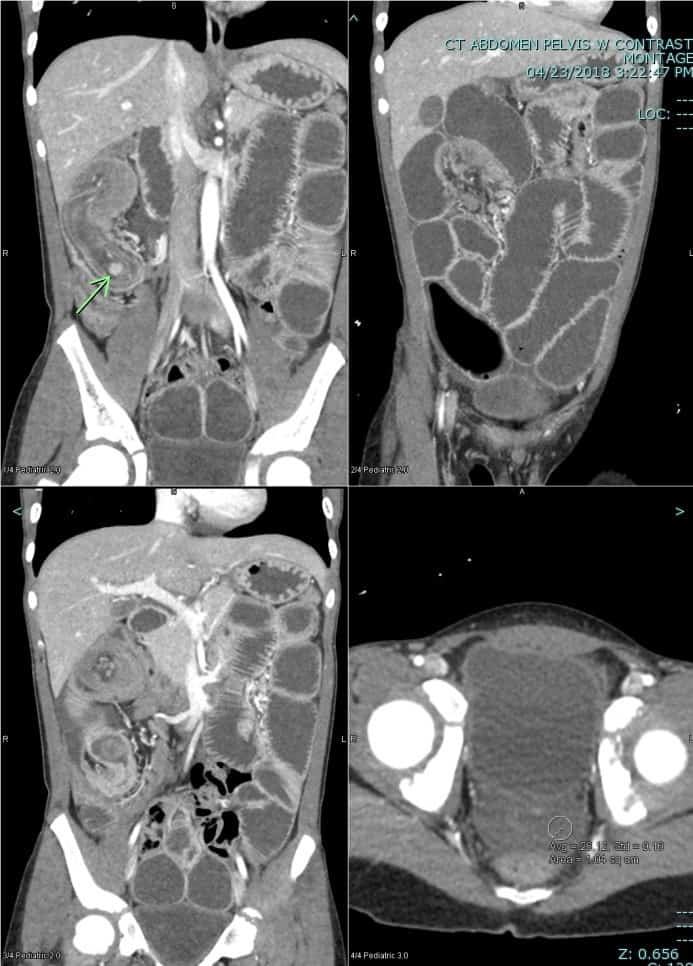
- An abdominal radiograph is obtained in the decubitus position to assess for free intraperitoneal air. A needle is always readily available in the room in case a need arises to decompress theabdomen.
- Lubricating jelly is applied and a small pediatric rectal tube/Foley catheter is inserted in the patient’s rectum and secured with tape.
- Instillation of air is then begun under intermittent fluoro until the intussusceptum is pushed back (intracolonic pressures are monitored to not exceed 120 mm Hg).
- Intussusception reduction is indicated by a sudden rush of air into the terminal ileum, sharp drop in the intraluminal pressures and is confirmed radiographically with dynamic overhead fluoroscopic imaging (8).

Keep in mind, a child sick for multiple days has higher risk of perforation before and during reduction — handle with care!
Selected References
1. Dunn EA, Olsen ØE, Huisman TAGM. The Pediatric Gastrointestinal Tract: What Every Radiologist Needs to Know. In: Hodler J, Kubik-Huch RA, von Schulthess GK, eds. Diseases of the Abdomen and Pelvis 2018-2021: Diagnostic Imaging – IDKD Book. Cham (CH): Springer; March 21, 2018.157-166.
2. S., L. B., Amar, G., & Ellen, P. (2017). Imaging of Pediatric Gastrointestinal Emergencies. Journal of the American Osteopathic College of Radiology, 6(1), 5–14. https://www.jaocr.org/articles/imaging-of-pediatric-gastrointestinal-emergencies
7. Mandeville, K., Chien, M., Willyerd, F. A., Mandell, G., Hostetler, M. A., & Bulloch, B. (2012). Intussusception: Clinical presentations and imaging characteristics. In Pediatric Emergency Care (Vol. 28, Issue 9, pp. 842–844). Pediatr Emerg Care. https://doi.org/10.1097/PEC.0b013e318267a75e
8. Vo, N. and Sato, T., 2020. Intussusception In Children. [online] Uptodate.com. Available at: <https://www.uptodate.com/contents/intussusception-in-children?search=intusscuception&source=search_result&selectedTitle=1~114&usage_type=default&display_rank=1#H14> [Accessed 2 August 2020].