Pyloric Stenosis
What is it?
Hypertrophic pyloric stenosis is the commonest acquired condition with an incidence of about 3 per 1,000 live births per year (10) in otherwise healthy neonates presenting with projectile non-bilious vomiting. Presenting between the sixth through twelfth weeks of life, Caucasian male first-born babies with a family history are the majority of the patient population (outnumbering females by 4 to 1) (2, 10).
How does it happen?
First there is idiopathic thickening of the circular muscular layer in the pylorus which results in the inability of the pyloric channel to relax and allow for the passage of gastric contents causing gastric outlet obstruction (GOO). It is often said that pyloric stenosis is the only clinical condition that can be felt (palpable “olive”) and seen (as waves of peristalsis traversing the midline) by the clinician (11).
What do I need to know?
Ultrasound is the ideal diagnostic modality for accurate, non-invasive and rapid confirmation of pyloric stenosis.
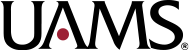
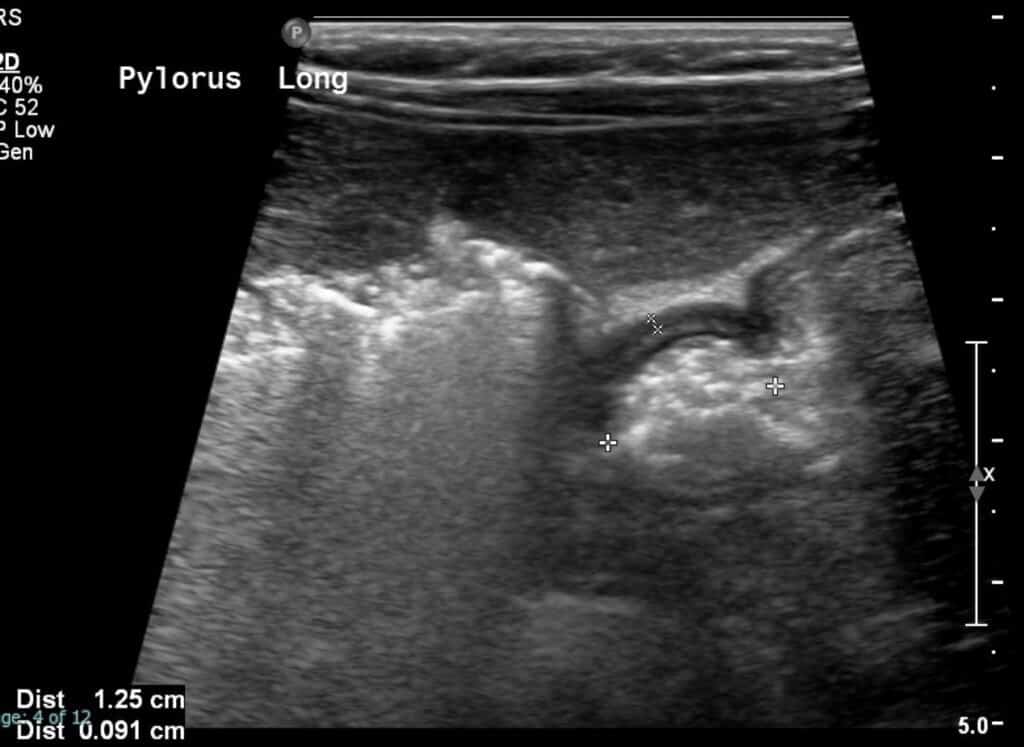
Sonographic findings demonstrate:
- Thickened hypoechoic muscular layer >3 mm in size
- On sagittal images, the thickened pylorus often resembles the appearance of the uterine cervix
- On transverse images, the thickened pylorus has targetoid pattern
- No passage of gastric contents through the pyloric canal
- Transverse pyloric diameter (wall to wall) >14 mm
- Abnormal elongation of the canal >15 mm in length
These important measurement values can be remembered by the mathematical “pi” sign (3.1415) where 3 represents the thickened muscular layer, 14 represents the transverse pyloric dimension and 15 represents the longitudinal measurement of the pyloric canal (12).
Cine grayscale images of the open pylorus demonstrate echogenic contents passing through the open pylorus. You may want to play the cine loop several times to appreciate this.

Cine sonographic images of the pylorus demonstrate pyloric canal elongation and thickening of the pyloric muscle with echogenic gastric content unable to pass through.
What do I need to do?
Pay attention to both cine and static images. The cine images should show echogenic food content unable to pass through the thickened pylorus. Report the dimensions of the pylorus displayed on the static images. Ask the tech to scan down lower to make sure you’re not missing a malrotated bowel if the pylorus looks normal. Basically you should have them scan the upper abdomen transversely in midline so you can look at the SMA/SMV orientation and for the whirlpool sign which may point toward a diagnosis of malrotation. You may want to hop on to read the article on malrotation to refresh your memory if needed.
Selected References
2. S., L. B., Amar, G., & Ellen, P. (2017). Imaging of Pediatric Gastrointestinal Emergencies. Journal of the American Osteopathic College of Radiology, 6(1), 5–14. https://www.jaocr.org/articles/imaging-of-pediatric-gastrointestinal-emergencies
10. Costa Dias, S., Swinson, S., Torrão, H., Gonçalves, L., Kurochka, S., Vaz, C. P., & Mendes, V. (2012). Hypertrophic pyloric stenosis: Tips and tricks for ultrasound diagnosis. In Insights into Imaging (Vol. 3, Issue 3, pp. 247–250). Springer. https://doi.org/10.1007/s13244-012-0168-x
11. Sharwood, E., 2020. Pyloric Stenosis. [online] Don’t Forget The Bubbles. Available at: <https://dontforgetthebubbles.com/pyloric-stenosis/> [Accessed 2 August 2020].
12. Muzio, B. and Qaqish, N., 2020. Hypertrophic Pyloric Stenosis (Ultrasound Measurements Mnemonic) | Radiology Reference Article | Radiopaedia.Org. [online] Radiopaedia.org. Available at: <https://radiopaedia.org/articles/hypertrophic-pyloric-stenosis-ultrasound-measurements-mnemonic-1?lang=us> [Accessed 2 August 2020].